September 2, 2024
Result Of Conjugated Estrogen In Stress Urinary Incontinence In Ladies With Menopause

Effect Of Conjugated Estrogen In Anxiety Urinary Incontinence In Ladies With Menopause The experience of frantically dripping pee can be an embarrassing problem for many people. Urinary incontinence is a loss of bladder control that's typically seen in older adults and women who have actually given birth or gone through menopause. Urinary system tract infections (UTIs), pelvic flooring disorders and an enlarged prostate are other causes. Estrogen and progesterone degrees raise continuously while pregnant and reach their height in the third trimester.
Medicines & Surgeries
Can hormonal agent discrepancy influence your bladder?

Exactly How Is Urinary System Incontinence Identified?
Hormone therapy (estrogen) in postmenopausal females alleviates urinary frequency and dysuria and blood circulation of bladder tissue boosts and brings about raise the toughness of muscular tissues around the urethra [44] Steroid hormones along with environmental effects in the urinary system system have a central function in the neural control of peeing procedure. Nevertheless, the specific mechanism of this action is unknown, yet the existence of both types of estrogen receptors in the brain cortex, limbic system, the hippocampus and the brain has been proved [36] Because of this, click here imipramine might serve for nighttime urinary incontinence. The most common side effects of anticholinergics are dry mouth and constipation. An extended-release type taken daily could trigger fewer side effects. The impact that HRT carries UI relies on the type of treatment carried out. Furthermore, the individual relearns just how to manage the bladder and reinforce the involved muscular tissues. Urinary system bladder hypocontractility or bad lodging of urine during storage space might lead to regular leakage of little volumes of urine. Dysfunction may be caused by urinary tract infection, chronic inflammatory conditions, neoplastic lesions, exterior compression, and chronic partial electrical outlet blockage. Additionally, females who are taking estrogen, if genital bleeding must refer doctor quickly. The RR for anxiety UI changed from 1.87 to 1.88, the RR for urgeUI changed from 1.15 to 1.13, and the RR for blended UI transformed from 1.49 to1.48. Change for parity in the regression models representing theestrogen alone trial did not alter any one of the RRs.- In those cases, your incontinence likewise generally stops once the problem is dealt with.
- In patients with dementia, urinary incontinence and urinary system dysfunction may result from specific participation of the locations of the cortex involved in bladder control.
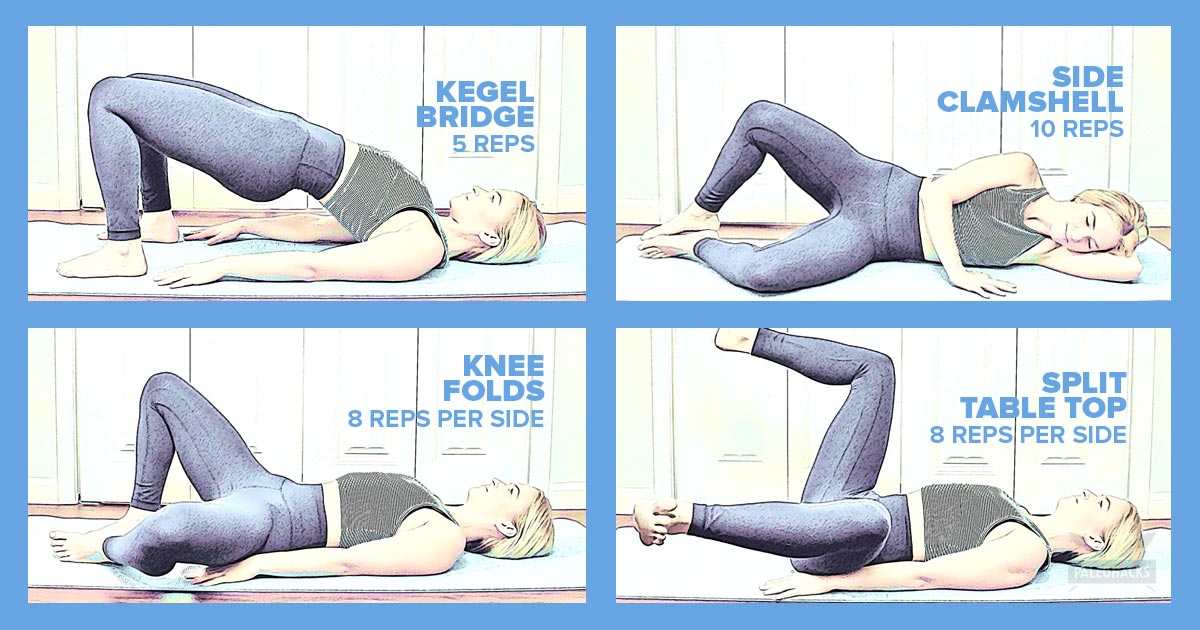
- Pelvic floor exercises (Kegels) can reinforce muscles and decrease symptoms.
Follow Mayo Clinic
These intermittent variants in urinary system routines emphasize the intricate interplay in between hormonal fluctuations and bladder function throughout the menstruation. Talk with your healthcare provider concerning these home treatment alternatives for urinary incontinence prior to starting any of them. You could not have the ability to treat all sorts of urinary incontinence with these way of living changes. Your company might likewise make thorough tips to you concerning the most effective way of living changes to try provided your incontinence medical diagnosis.Social Links