Tension Incontinence: Causes, Signs And Treatment

Estrogen
According to the National Organization for Continence, over 25 million adult Americans experience momentary or persistent urinary system incontinence. UI can take place at any type of age, yet it is extra typical amongst women over 50. Urinary system incontinence may be a short-term condition that results from a hidden medical problem. It can range from the discomfort of small losses of urine to extreme, regular wetting. Whether experiencing hormonal adjustments throughout puberty, menstrual cycle, maternity, or menopause, ladies can gain from INNOVO's non-invasive and scientifically tried and tested technique to pelvic flooring conditioning.Dealing With Urinary Problems With Innovo
These intermittent variations in urinary system practices highlight the intricate interplay between hormonal fluctuations and bladder function throughout the menstrual cycle. Talk to your healthcare provider regarding these home treatment options for urinary incontinence before starting any of them. You may not be able to treat all kinds of urinary incontinence with these way of life changes. Your company might additionally make in-depth ideas to you concerning the most effective way of living adjustments to attempt given your incontinence diagnosis.Exactly How Can I Reduce My Danger Of Anxiety Urinary Incontinence?
Keeping a healthy body weight can likewise help with bladder control. Talk to your doctor about the most effective means to preserve strong pelvic flooring muscle mass throughout your life. Inexperience of the urethral sphincter system (urethral smooth/striated muscle, connective tissue) may arise from nonneurogenic diseases (bladder, urethra, prostate gland) or neurogenic reasons.- The psychosocial expenses and morbidities are even more challenging to measure.
- Your health care supplier could recommend repeating the shots one or two times a year.
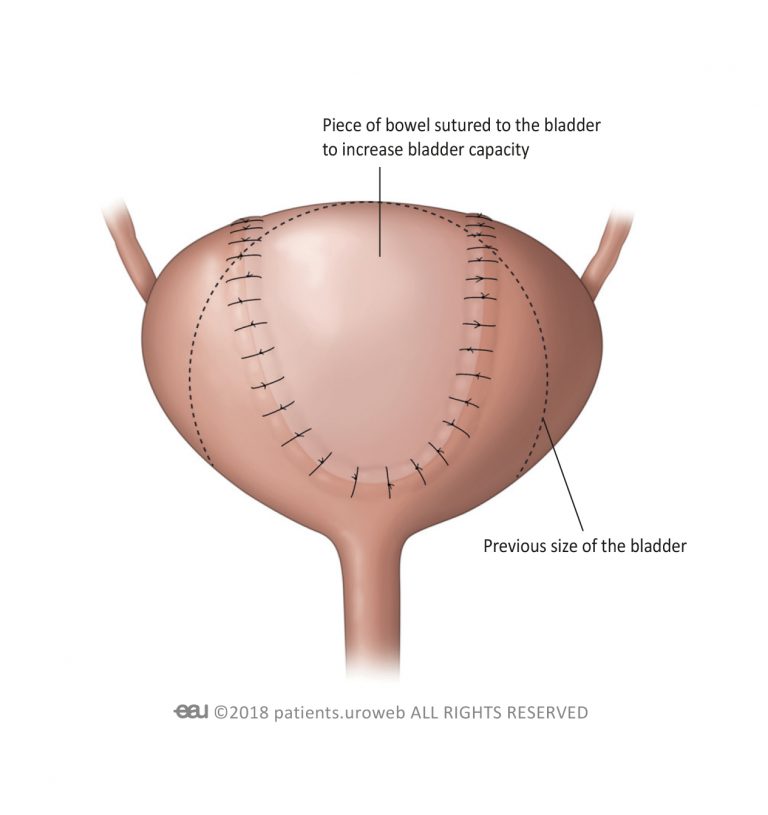
- The maximal storage capability of the bladder is reached, often without the individual recognizing that this has taken place.
- One of the most usual hereditary problems creating urinary incontinence consist of ectopic ureter( s), and related structural abnormalities (license urachus, pseudohermaphrodites, and urethrorectal fistulae).
Exactly how to treat hormonal agent inequalities?
hormonal agent (PTH) and calcitonin. Quit smoking. If you smoke, you put yourself in jeopardy of urinary incontinence, since coughing places pressure on your pelvic flooring muscles.Do the appropriate exercises.Avoid lifting.Lose excess weight.Treat bowel irregularity promptly.Cut down on caffeine.Cut down on alcohol.Drink plenty of water. Ideal fruits: apples, bananas, blackberries, coconut, grapes, strawberries and watermelon.Best vegetables: asparagus, broccoli, carrots, celery, cucumbers, kale, lettuce and peppers.Best fibre-rich foods: almonds, artichoke, barley, beans, bran, lentils, oats and raspberries. One aspect that has actually acquired substantial attention as a reason for urinary system incontinence is reduced estrogen. Estrogen, a hormone largely associated with reproductive health, plays