September 13, 2024
Ppt Incontinence In Older Grownups: Going Beyond The Bladder Powerpoint Discussion Id:3022076
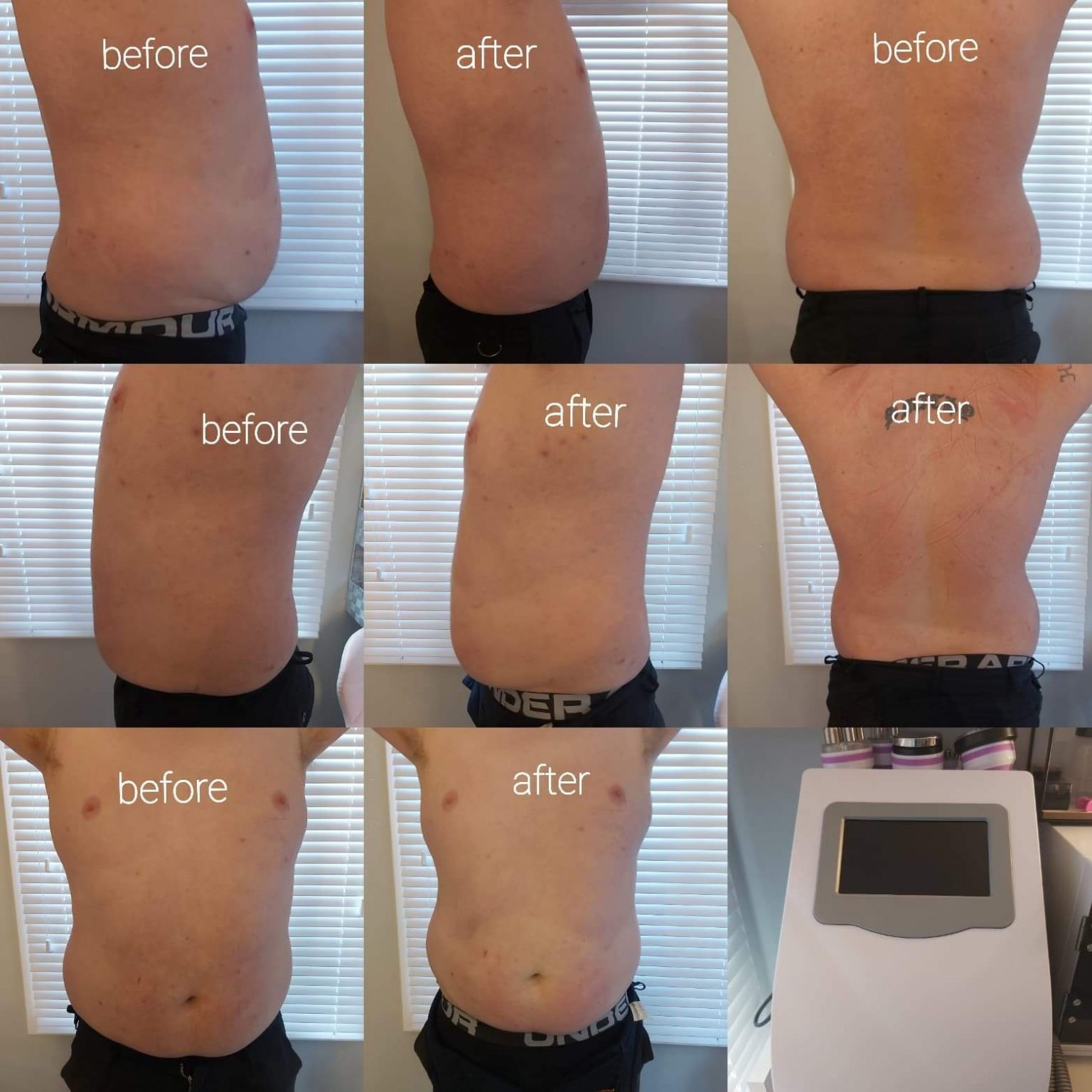
Electromuscular Excitement For Urinary System Incontinence: Levator 100 " A significant variety of people are looking for stronger core muscle mass and not simply looking great in their bikini or summertime clothes. Many have back problems and/or urinary incontinence and are preferring a stronger core to reduce these issues," Dr. Covey states. Contraction of the outside penile muscle mass, ischiocavernosusmuscle, and bulbospongiosus muscular tissue, which become part of the malepelvic flooring, causes enhanced stress in the corpuscavernosum. It is essential to locate an equilibrium in thesuitable treatment of ED entailing PFM. The Burch procedure, the most usual suspension surgical procedure, adds assistance to the bladder neck and urethra, decreasing the risk of tension incontinence.- Therapy includes inserting a small needle, affixed to a stimulant, in the ankle joint.
- Right patient selection is vital for the treatment to succeed.
- Postoperative infection prices range 2% and 3%. and are increased in patients with a history of pelvic radiation.
- For boosting ED, pharmacotherapy withdrugs based on blood supply enhancement prevails [19-22] However, the efficiency relies on the root cause of ED and overtime might decline due to modern damages to little bloodvessels [23]
- The result of an audit of using the Levator 100 EMS tool, the forerunner to the newer Levator Turbo CS200, is examined.
- Sterile draping should fit cystoscopy followed by gadget positioning.
Urinary Incontinence
Throughout the therapy, the patient is totally outfitted, andthat contributes to higher convenience, getting over shyness, andbetter individual compliance. The goal of this pilot research study is toassess the security and performance of HIFEM technology fortreating male UI with ED utilizing this ingenious gadget andchallenge the stigma bordering intimate male wellness problems. The Emsella therapy is entirely painless, non-invasive, and convenient. As you sit and take in the electro-magnetic power of the chair on your pelvic floor, you might experience prickling in the pelvic flooring due to the contraction.Electromuscular Stimulation For Urinary System Incontinence: Levator 100
The dental implant should be put with the mesh backing facing the outside and the blow up side facing the urethra. Pass the cuff tubing with the opening in the mesh with a right-angle clamp, locking the system around the urethra and guaranteeing that the mesh securing device is seated safely until the tab can be pulled over the tubes adapter. To prepare the pressure-regulating balloon, prepare a 30-mL syringe with 25 mL of filling up service and affix a 15-gauge blunt needle. The first choice is to push down on the deactivation switch for a few mins to enable some liquid to leak from the pressure-regulating balloon into the pump and permit a switch of the shutoff into the open position. The second alternative is to make use of a very narrow instrument, such as the suggestion of a hemostat or the rear of a cotton-tipped applicator, to manually press the piston open on the precise opposite side of the deactivation switch. Patients may need a local anesthetic due to the sensitivity of this location. As soon as this is full, use fluoroscopy to picture the balloons. The black tubing attaches to the balloon reservoir, and the clear tubes attaches to the cuff. When the connections have actually been approximated, cut any excess tubes to make the most of individual comfort. To connect the tubes, put the collet owner into the tubing; the collet owner has a number of collets on it. Balloon tanks are readily available in 5 series of water pressure measured in centimeters of water (cm H2O). Available arrays are 41 to 50, 51 to 60, 61 to 70, 71 to 80, and 81 to 90 centimeters water. While submerged, lightly clamp the tubing 4 to 5 centimeters from its end utilizing a rubber-shod hemostat. The AUS advertises urinary system continence using circumferential compression of the urethra. If the individual finds that the gadget is not functioning after placement, a physical exam is required; imaging might be required. It is recommended to work through the complying with steps when troubleshooting an AUS. If the client never ever accomplishes continence after AUS activation, one of the most common causes are either the dental implanted cuff is as well huge or the reservoir has inadequate pressure. The most usual virus are Staphylococcus aureus and Streptococcus epidermidis. The AUA advises prophylactic antibiotic therapy with vancomycin to alleviate this threat. If individuals establish signs of infection, instant elimination of the gadget is required. Indications of infection include pain at the pump site, erythema, edema, and purulent discharge. As soon as in the appropriate anterior-posterior aircraft and through the urogenital diaphragm, position the trocar lateral to the urethra and distal to the bladder neck. The power resources may be a mechanical device (ie, a lithoclast [pneumatically-driven jack hammer], an ultrasonic tool, an electrohydraulic tool, a hand-operated lithotrite, or a laser. Radiographic studies can be a beneficial analysis tool if contrast was initially used as a filling up liquid. When non-active or open, comparison ought to show up in the pump and the storage tank but not in the cuff. When active or closed, a ring of comparison need to be visible at the cuff site. If the device stays nonoperational after fixing, a cystoscopy is advised to assess the cuff. The locking device does not have responsive comments, and it can be testing to determine if the device is open or secured. Compression on both sides of the locking switch will certainly enable some fluid to return to the pump and bypass the delayed-refill resistor system. Unintended peritoneal entrance and digestive tract injuries have been reported. A digestive tract opening would certainly need an immediate repair work and deserting the fabricated sphincter implantation treatment. In a clean and sterile style, fill up the syringe with 2 mL of regular saline making use of the 18-gauge needle and exchange this for the 23-gauge needle. The carrying out specialist should stand on the side of the client opposite their dominant hand. Nonetheless, a tube that is as well long might develop kinks that can impair normal device procedure. Using kinkproof tubing has actually considerably reduced this complication, particularly after 3 months postimplantation of the tool. Urinary retention in the initial 24 hours after AUS positioning can be managed with a Foley catheter. If the retention lasts more than 48 hours, a suprapubic catheter can be positioned to help with bladder drain. If the retention lingers, the urethral cuff may be too small and call for modification. Relying on the extent of urinary leak, 0.5 to 1.0 mL per balloon can be added at one time.Can incontinence be treated in older adults?
Sensors
Electrical nerve excitement sends out light electric currents to the nerves around the bladder that help control peeing and your bladder''s reflexes. Surgery can in some cases boost or cure incontinence if it is triggered by a modification in the placement of the bladder or blockage due to an enlarged prostate.
Social Links