September 7, 2024
Solutions For Your Urinary System Incontinence: Melissa Grier, Md: Obgyn
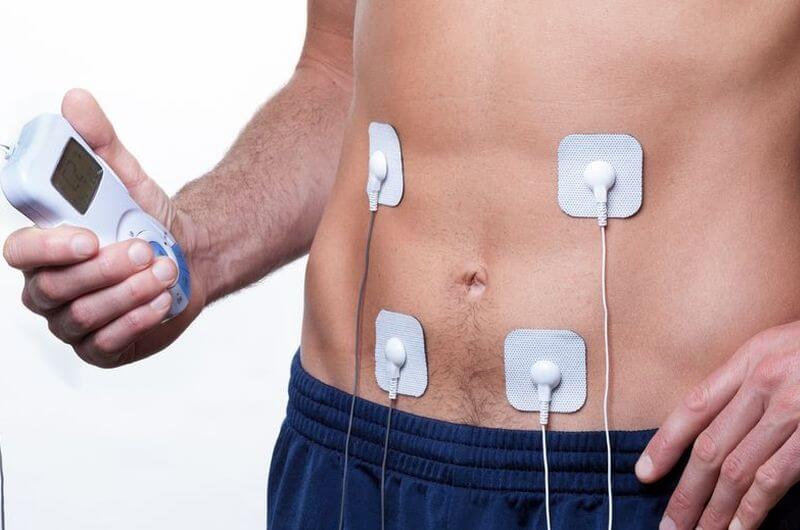
Hormonal Agent Modifications In Females Your pelvic flooring muscle mass may also deteriorate with age and less physical activity. The professional might be a urologist, that deals with urinary system problems in both males and females, or a urogynecologist, who has special training in the women urinary system. You may also require to see a pelvic floor professional, a sort of physical therapist, who will collaborate with you to reinforce your pelvic flooring muscular tissues that support the urinary system system. The differentiating features of practical incontinence include the lack of bladder dysfunction; rather, it is defined by the lack of ability to take care of urination because of exterior variables. For example, a female might understand she needs to make use of the washroom yet can not get there swiftly sufficient as a result of physical restrictions or complication. Anxiety urinary incontinence happens when exercises like coughing or sneezing put pressure on the bladder, while desire urinary incontinence is identified by an abrupt, intense impulse to urinate.Electrical Stimulation-- An Actual Option For Combined Incontinence
The frequency of stress incontinence comes to a head in the 5th decade and after that declines, whereas the occurrence of both combined and seriousness urinary incontinence continues to raise with age. Empirical information are from France, Germany, Spain and the United Kingdom180. Mean frequency information from an evaluation of epidemiological research studies from around the world have actually shown comparable trends22. Blended incontinence is a sort of urinary incontinence that takes place when a specific experiences a combination of stress and anxiety incontinence and advise urinary incontinence.Medicines And Hormonal Agent Therapy
During your consultation, Dr. Grier may run an urine test, as well as a special test to gauge your pee outcome. She might additionally ask you to maintain a bladder journal for an amount of time to track your signs and symptoms. If you have urinary system incontinence, you can make a consultation with your primary care supplier, your OB/GYN, or a nurse expert. Your doctor or registered nurse will certainly work with you to treat your urinary incontinence or refer you to an expert if you need various therapy. Menopause-related urinary incontinence can be efficiently managed with a range of therapy choices. These options can be categorized into way of life and behavioral modifications, medical interventions, and alternative therapies. At Melissa Grier, MD Female's Healthcare in Pasadena, California, Dr. Grier, and her group provide the minimally invasive treatment, Viveve ®, to soothe your symptoms and bring back your comfort. Take a few minutes to learn more about urinary system incontinence, including services to take into consideration. If urinary incontinence is impacting your life, the best thing you can do is see your physician. Schedule an assessment with your Florida Female Treatment of Jacksonville OB/GYN. We will analyze you and help offer the guidance you require to find the reason for your urinary incontinence and treat it. An obstruction along your urinary tract can block your body's all-natural disposal.What vitamin stops over active bladder?
Vitamin D supplementation may be gaining acknowledgment as a reliable technique for avoidance or alleviation of bladder symptoms such as overactive bladder and urinary incontinence.
- As necessary, the medicine is not suggested as first-line therapy59,76, and determination of use for the indicator of urinary incontinence is poor144; thus it is not generally utilized.
- A few of these drugs can be quite costly as not every one of them are available on the Drug Advantages System (PBS).
- Difficulties might include anything from a boost in UTIs to development of a bacterial skin infection called cellulitis.
- Managing menopause incontinence in the house includes techniques like Daily Techniques for Handling Leak, Use of Absorbent Products, and Producing an Encouraging Home Setting.
Social Links