September 8, 2024
Urinary System Incontinence In Ladies: Types, Therapies, And Expectation
Whats The Treatment For Urinary System Incontinence In Females? Mixed urinary incontinence is a typical kind of urinary system incontinence that many ladies experience during menopause, incorporating components of both anxiety and urge urinary incontinence. This condition can materialize as involuntary leakage during physical activities, such as coughing or sneezing (anxiety incontinence), in addition to an unexpected, strong impulse to urinate that might result in leak (desire incontinence). The reasons for blended incontinence during menopause are commonly multifactorial, involving hormone modifications that damage pelvic floor muscles, age-related bladder changes, and the advancing impacts of giving birth. Way of living aspects, such as high levels of caffeine and alcohol consumption, can significantly influence urinary incontinence in menopausal women. Caffeine, located in coffee, tea, and some sodas, is a diuretic that can enhance pee manufacturing and aggravate the bladder, bring about even more constant urination and seriousness. Alcohol can unwind the bladder muscular tissue, impairing its capacity to agreement successfully and increasing the threat of leak.- Adding in anticholinergic drugs can help along with bladder training and weight management.
- Ins( 1,4,5) P3, inositol 1,4,5-trisphosphate; PKA, protein kinase A; PKC, protein kinase C; PKG, protein kinase G; NO •, nitric oxide; NOS, NO synthase.
- Both most usual kinds of urinary incontinence that affect ladies are stress and anxiety incontinence and advise urinary incontinence, likewise called overactive bladder.
- As an example, your physician might prescribe anticholinergics to calm your bladder if it's overactive.
Treatment Alternatives
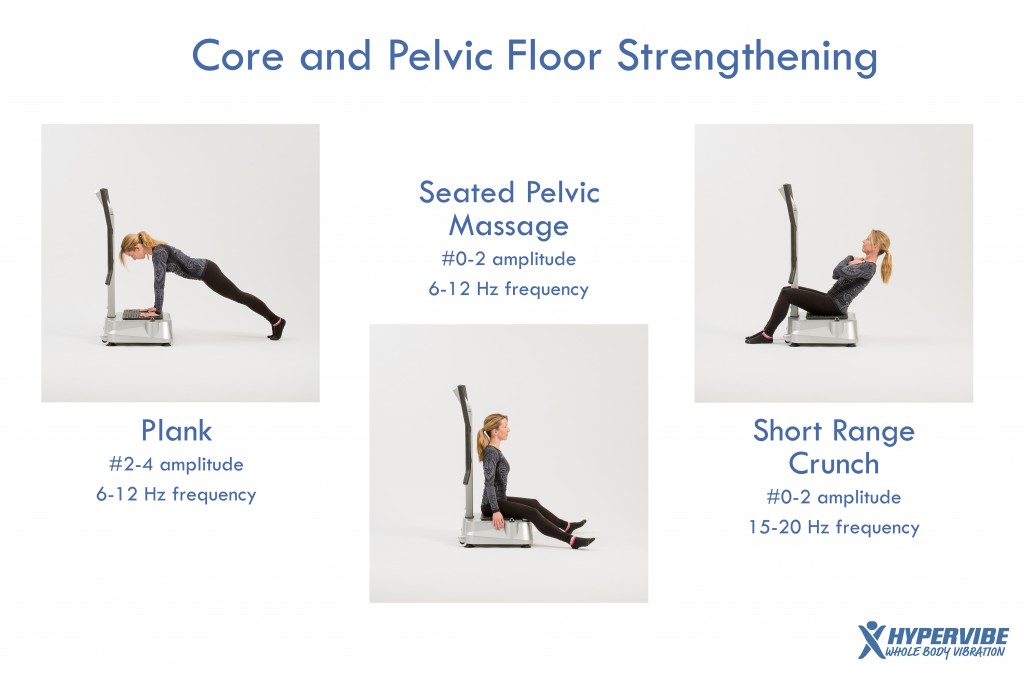
From occasional, minor leakages, to more constant spells of crashes, the sort of urinary incontinence you experience can lose extra light on its root cause and just how to treat it. If you are awkward or unpredictable about doing Kegel workouts by yourself, a doctor or nurse can also teach you just how to do Kegels. A pelvic floor physical therapist or various other professional may likewise be readily available in your area to aid instruct you how to strengthen these muscles.Choosing The Appropriate Female External Urinary Catheter For Home
Some ladies have urinary system signs and symptoms since the pelvic floor muscular tissues are always tightened. In this scenario, Kegel exercises will not assist your urinary symptoms and may create much more troubles. Speak to your physician or registered nurse about your urinary system signs before doing Kegel workouts. Urinary system urinary incontinence is normally caused by troubles with the muscular tissues and nerves that assist the bladder hold or pass pee. Specific wellness events unique to females, such as pregnancy, childbirth, and menopause, can trigger issues with these muscular tissues and nerves. In a female with typical bladder function, the muscle mass of the pelvic flooring contract when she is doing any kind of exercises. Both sphincters assist to block the urethra to preserve continence. In some cases, there are modifications to your day-to-day life that can in fact aid your urinary incontinence. These modifications usually include exercises you can do to reinforce your pelvic flooring muscles, changes to your typical routines and an improved diet regimen. Some people notice improvements by making these modifications at home and don't need extra therapy. 4 in 10 women boosted their signs and symptoms after attempting Kegels.9 Kegels can be done daily and may be especially helpful while pregnant. They can aid avoid the weakening of pelvic flooring muscular tissues, which usually happens while pregnant and childbirth.What sort of hormonal agent treatment can treat urinary incontinence?
Numerous researches have actually demonstrated that oestrogen replacement can improve, or perhaps treat, urinary system stress and anxiety and urge urinary incontinence.
Social Links