
September 3, 2024
Tension Incontinence: Causes, Signs And Treatment

Urinary System Incontinence
You might experience leak for a wide variety of reasons-- typically depending on the kind of urinary incontinence you have. There are no alternative medication therapies that have actually been confirmed to cure urinary incontinence. Very early researches have shown that acupuncture can offer some advantage. Yoga likewise may supply some advantage for urinary incontinence, however extra study is required. To help you identify and contract the ideal muscle mass, your medical professional may suggest that you work with a pelvic flooring physiotherapist or attempt biofeedback techniques. Since we understand progesterone levels increase after ovulation, it's suggested that these high degrees of the hormone might create an uptick in detrusor task. For ladies experiencing SUI, everyday tasks can become resources of anxiety and shame, leading to a significant decrease in their lifestyle. Nonetheless, with the appropriate intervention and assistance, it is possible to strengthen the pelvic floor muscle mass and gain back control over urinary feature. Pregnancy stands for a period of profound hormonal changes as the body undertakes amazing adaptations to sustain fetal development and advancement. Estrogen and progesterone levels climb exponentially, promoting uterine development and preparing the body for giving birth. Nonetheless, these hormonal shifts can likewise impact the pelvic floor muscles, resulting in urinary concerns during pregnancy and postpartum.How can bladder leakage be quit?
and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and rest issues.Digestive distress. Using low-dose, topical estrogen might aid. The drug comes in the form of a vaginal lotion, ring or spot. The estrogen might aid recover the cells in the vagina and urinary tract to eliminate some symptoms. Topical estrogen may not be risk-free for individuals with a background of bust cancer cells, uterine cancer or both. Recap. Bladder disorder is an usual challenge, especially later on in life and during times of significant hormonal adjustment. Reduced estrogen bladder signs can include incontinence, over active bladder, and pain.
How To Handle Urinary Incontinence And Reduced Estrogen
Urinary system incontinence might occur on its own or might be accompanied by various other unclear neurological signs and symptoms. Spinal cord lesions can alter supportive and parasympathetic tone, resulting in urinary incontinence. Outer nerve disease such as diabetic peripheral neuropathy can create urinary incontinence with a contractile disorder of the bladder. It's considered for people that can't be helped by various other types of therapy. Electric stimulation of your pelvic muscles may help your regain control of your bladder if your UI is related to nerve problems. Your medical professional may also suggest more engaged therapy alternatives, specifically if they don't think that way of living adjustments are aiding. Botulinum contaminant (Botox) in some cases is infused into the bladder muscles to alleviate muscle convulsions. Urinary system urinary incontinence typically goes unreported for years due to the fact that several females are either humiliated, by the condition or believe there is no remedy.- Although information worrying urinary incontinence in individuals of various races are sparse, records are emerging that race might play an important function in the prevalence and probability of reporting of urinary incontinence.
- On top of that, urinary system incontinence is underdiagnosed and underreported.
- An extensive neurologic examination should be executed in an attempt to establish or rule out a neurogenic reason.
- It might lead to more frequent urination, pain throughout sex, vaginal dry skin, and other symptoms.
- Pets with outer nerve damages adequate to create LMN problems of micturition usually have LMN deficiencies in the perineal area (lowered anal sphincter tone).
What Is Incontinence?
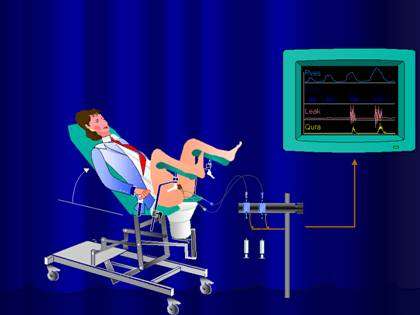
First-line administration consists of way of living and behavior modification, pelvic flooring workouts and bladder training. Estrogens and various other pharmacological interventions are practical in the treatment of necessity urinary incontinence that does not reply to conservative actions. Third-line therapies (e.g. sacral neuromodulation, intravesical onabotulinum toxin-A shots and posterior tibial nerve stimulation) are useful in selected clients with refractory urge urinary incontinence. Urinary incontinence is the Fluid management uncontrolled leak of urine, and there are several possible causes. If you are thinking about hormonal agent therapy, examining the prospective threats and advantages independently with your healthcare provider is necessary. Nerve damages can disrupt signals from your bladder to your mind so you don't experience the urge to urinate. Urinalysis may reveal proof of urinary tract infection (bacteriuria, inflammatory pee debris) or be helpful of a polyuric disorder (reduced urine-specific gravity). Urodynamic treatments such as urethral pressure profiles, cystometrography, and electromyography may be taken into consideration to analyze bladder, urethral, and neurologic function in even more deepness. Urinary system incontinence is specified as spontaneous loss of pee from the urinary system.Social Links