Effects Of Estrogen With And Without Progestin On Urinary System Incontinence Geriatrics Jama
Impact Of Conjugated Estrogen In Anxiety Urinary System Incontinence In Women With Menopause Comparing volunteer and spontaneous urination is essential to the analysis plan. 3 kinds of lesion of disintegration, ectropion and cervical lesions in post-me- nopause is seen extra. Endocervix glandular cells task throughout menopause and subsequently the amount of mucin decreases that this triggers to genital dryness that emerges as a main complaint in postmenopausal ladies. Mild electrical stimulation can be effective for stress incontinence and prompt urinary incontinence, but you may need multiple treatments over a number of months. Obstructive disorders should be handled as swiftly as feasible. Urinary system infection should be treated with suitable clinical treatment. Ectopic ureters and other congenital abnormalities can be surgically remedied; the medical professional should realize that functional irregularities of urinary system bladder storage space or urethral proficiency may accompany this flaw.Therapies
These hormone shifts can influence bladder feature and urinary routines, showing up as urinary system symptoms such as enhanced frequency, seriousness, or leakage. Low levels of estrogen and urinary system incontinence go together. As ladies age and start coming close to menopause, the ovaries decrease the procedure of making estrogen, and the levels of this female sex hormone naturally decrease in the body. [newline] At some point, with menopause, the production of estrogen quits, and this impacts the body in numerous ways. Without estrogen, females locate it challenging to preserve healthy urologic functions throughout and after menopause. Bladder control for ladies starts alongside their last menstrual period and boosts thereafter.Addressing Urinary Issues With Innovo
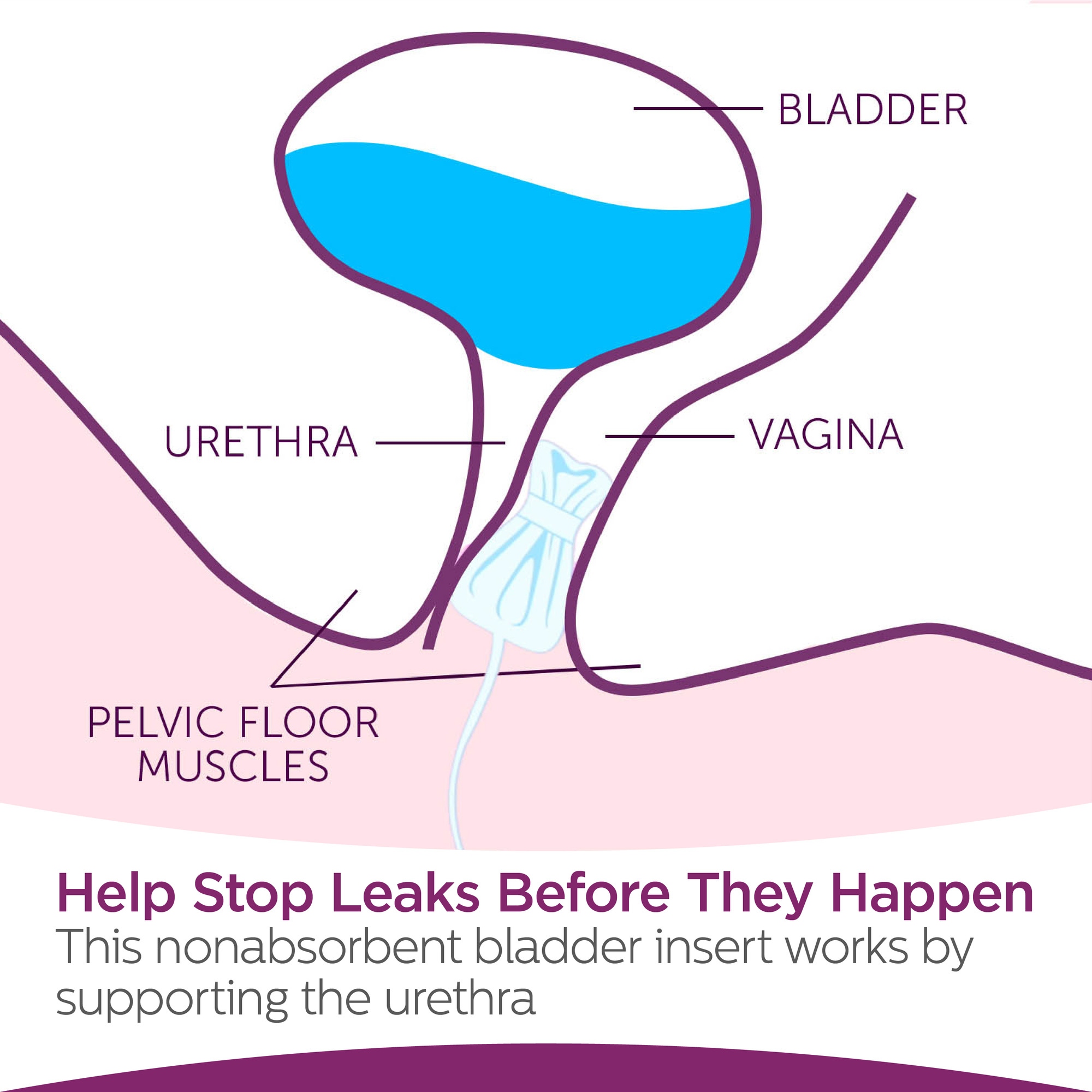
Urethral incompetence normally causes intermittent urinary incontinence, typically at remainder. Hormonal agent treatment (estrogen) in postmenopausal ladies minimizes urinary regularity which results in increase in the toughness of muscles around the bladder. Althoughbasic science in this field is restricted, a recent placebo-controlled, randomizedclinical test of estrogen alone sheds light on this problem. Urethral closureis based on the integrated activity of the suburethral vaginal wall, thepubourethral ligaments, the pubococcygeus muscles, and the paraurethral connectivetissues. As Stress Incontinence you age, the muscle mass that support your pelvic organs can damage. This indicates that your bladder and urethra have less assistance-- typically resulting in pee leakage.Pelvic Flooring Exercises
Throughout this procedure, the posterior wall of the urethra shears off the anterior urethral wall surface to open up the bladder neck when intrinsic sphincter deficiency exists. Practical incontinence is the failure to hold urine because of reasons other than neuro-urologic and lower urinary system tract dysfunction. Videourodynamic researches are scheduled to assess intricate cases of stress urinary incontinence.- Double-contrast cystography may be suggested for complete visualization of the urinary system bladder and identification of urinary bladder lesions.
- Endocervix glandular cells activity during menopause and subsequently the quantity of mucin decreases that this creates to vaginal dry skin that occurs as a major grievance in postmenopausal women.
- Advise urinary incontinence is a lot more widespread after the menopause, and the top frequency of tension incontinence takes place around the moment of the menopause.
- These hormone shifts can affect bladder feature and urinary practices, materializing as urinary system signs such as boosted regularity, seriousness, or leak.
- Tension urinary incontinence creates when activity places boosted stress on your bladder.
How to deal with hormonal agent imbalances?
hormonal agent (PTH) and calcitonin. Stop cigarette smoking. If you smoke, you put on your own in danger of urinary incontinence, because coughing puts pressure on your pelvic floor muscles.Do the ideal exercises.Avoid lifting.Lose excess weight.Treat irregularity promptly.Cut down on caffeine.Cut down on alcohol.Drink plenty of water. Best fruits: apples, bananas, blackberries, coconut, grapes, strawberries and watermelon.Best veggies: asparagus, broccoli, carrots, celery, cucumbers, kale, lettuce and peppers.Best fibre-rich foods: almonds, artichoke, barley, beans, bran, lentils, oats and raspberries. One element that has actually gotten considerable interest as a source of urinary incontinence is low estrogen. Estrogen, a hormonal agent mainly connected with reproductive wellness, plays