
September 3, 2024
The Effect Of Hormone Treatment On Urinary Incontinence Incontinence Institute
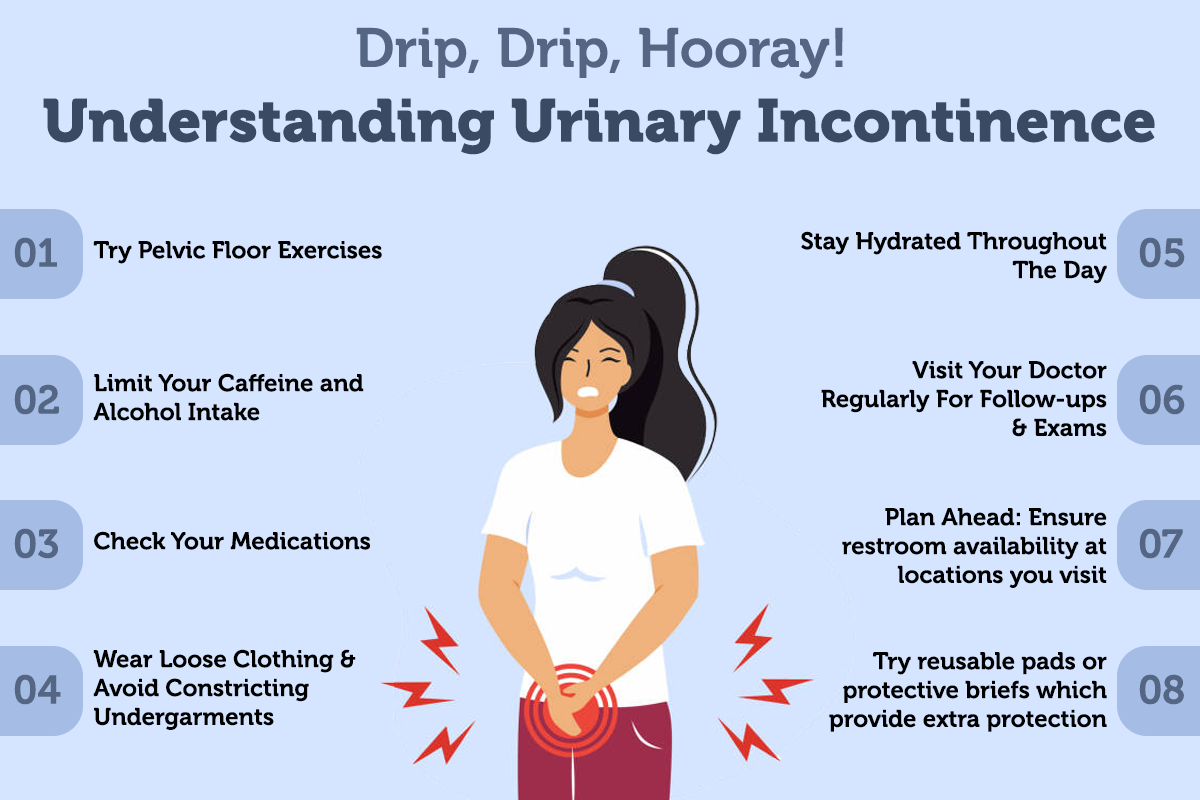
6 Means To Deal With Bladder Leak Throughout a lady's life, from puberty to menopause, the fragile balance of hormonal agents manages a symphony of changes that can impact urinary system continence and pelvic floor stamina. Occasionally, there are adjustments to your day-to-day life that can in fact aid your incontinence. These modifications usually consist of workouts you can do to enhance your pelvic floor muscular tissues, adjustments to your normal habits and an improved diet. Some people discover enhancements by making these modifications in the house and do not require additional treatment. By integrating INNOVO into their treatment plan, ladies can support their urinary system health and wellness and gain back self-confidence in their lives. Kegel workouts are a simple method to construct strength in your pelvic floor muscle mass. These exercises are done by lifting, holding and afterwards unwinding your pelvic flooring muscle mass. You can locate these muscular tissues by quiting the flow of urine mid-stream while you're peing. Only do this up until you learn exactly how to locate the muscle mass-- stopping the circulation of pee mid-stream isn't healthy over a long period of time.Desire Urinary Incontinence Pathophysiology
These hormone shifts can influence bladder function and urinary routines, manifesting as urinary signs and symptoms such as enhanced regularity, urgency, or leakage. Reduced degrees of estrogen and urinary incontinence go hand in hand. As females age and start approaching menopause, the ovaries reduce the procedure of making estrogen, and the levels of this women sex hormone naturally decrease in the body. [newline] At some point, with menopause, the production of estrogen stops, and this affects the body in many means. Without estrogen, women discover it difficult to maintain healthy urologic features throughout and after menopause. Bladder control for females starts alongside their last menstruation period and increases thereafter.Dealing With Urinary System Concerns With Innovo
If directed to seek surgical treatment by your medical professional, prompt action is encouraged, as waiting may minimize the efficiency of surgical therapy. The point of views shared in person endorsements are by patients only; they are not qualified medical professionals. These point of views ought to not be relied upon as, or in place of, the medical suggestions of a qualified medical professional, etc. Urinary incontinence is a prevalent condition influencing many individuals, particularly postmenopausal ladies. Subject estrogen products may additionally help to tone your urethra and vaginal areas. Electrical treatments are used directly over the pelvic flooring muscular tissues. Biofeedback to enhance and coordinate the pelvic flooring muscular tissues. Psychophysiological feedback is coordinated with pelvic flooring (Kegel) exercises. Alpha-adrenergic agonists might be administered for the management of urethral inexperience, alone or in combination with reproductive hormonal agents, where a synergistic result is occasionally observed.- Endocervix glandular cells task during menopause and subsequently the amount of mucin decreases that this causes to genital dryness that emerges as a major grievance in postmenopausal women.
- In biofeedback, a cable is linked to an electric spot over your bladder and urethral muscle mass.
- Urge urinary incontinence is more prevalent after the menopause, and the top frequency of stress and anxiety urinary incontinence happens around the moment of the menopause.
- These hormonal changes can influence bladder function and urinary system behaviors, showing up as urinary signs and symptoms such as raised frequency, urgency, or leakage.
- Stress and anxiety urinary incontinence develops when task places boosted pressure on your bladder.
What hormone maintains you from peeing?

Social Links