September 1, 2024
Effects Of Estrogen With And Without Progestin On Urinary System Incontinence Geriatrics Jama
Desire Incontinence Pathophysiology
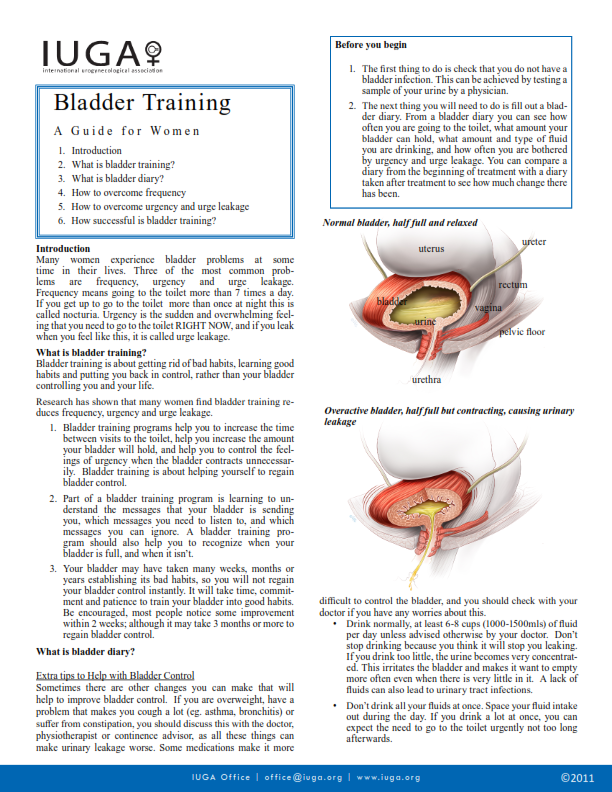
These hormone shifts can affect bladder feature and urinary behaviors, manifesting as urinary signs and symptoms such as raised frequency, urgency, or leakage. Reduced levels of estrogen and urinary incontinence go hand in hand. As women age and start approaching menopause, the ovaries decrease the procedure of making estrogen, and the levels of this female sex hormonal agent normally decrease in the body. [newline] At some point, with menopause, the production of estrogen stops, and this affects the body in lots of means. Without estrogen, ladies locate it challenging to maintain healthy urologic functions during and after menopause. Bladder control for women starts alongside their last menstrual duration and increases thereafter.How Is Urinary Incontinence Treated?
These intermittent variations in urinary routines highlight the elaborate interaction between hormone variations and bladder function throughout the menstruation. Speak to your healthcare provider regarding these home treatment options for urinary incontinence prior to beginning any one of them. You could not be able to treat all types of urinary incontinence with these way Bladder control of life modifications. Your company could additionally make comprehensive pointers to you regarding the most effective way of living changes to attempt offered your incontinence medical diagnosis.How Is Stress Urinary Incontinence Identified?
It also assists maintain your bladder and urethra healthy and working correctly. They may no longer be able to regulate your bladder as they did previously. As your estrogen levels continue to go down throughout and after menopause, your UI signs and symptoms may worsen. Estrogens, typically in the type of diethylstilbestrol, are carried out to purified ladies.- Endocervix glandular tissue activity during menopause and ultimately the quantity of mucin reduces that this creates to vaginal dryness that occurs as a primary complaint in postmenopausal females.
- Urge urinary incontinence is more prevalent after the menopause, and the top frequency of tension incontinence occurs around the time of the menopause.
- These hormone shifts can influence bladder feature and urinary habits, materializing as urinary system signs and symptoms such as boosted regularity, necessity, or leak.
- Stress incontinence establishes when activity places enhanced pressure on your bladder.
Which hormone is accountable for bladder?
Social Links