September 10, 2024
Management Of Urinary System Incontinence In Postmenopausal Women: An Emas Clinical Overview
Impact Of Conjugated Estrogen In Stress Urinary System Incontinence In Females With Menopause Throughout a woman's life, from adolescence to menopause, the delicate balance of hormonal agents manages a symphony of adjustments that can affect urinary system continence and pelvic floor stamina. Occasionally, there are changes to your daily life that can really aid your incontinence. These adjustments often include exercises you can do to reinforce your pelvic flooring muscular tissues, changes to your normal practices and a boosted diet plan. Some people discover renovations by making these changes in the house and don't require extra treatment. Hormonal agent treatment (estrogen) in postmenopausal women reduces urinary regularity and dysuria and blood flow of bladder tissue rises and causes enhance the stamina of muscles around the urethra [44] Steroid hormones in addition to ecological effects in the urinary tract have a main role in the neural control of peeing process. However, the precise mechanism of this action is unidentified, but the presence of both kinds of estrogen receptors in the mind cortex, limbic system, the hippocampus and the cerebellum has actually been shown [36]Urinary System Disorders
These hormonal changes can affect bladder function and urinary system habits, manifesting as urinary system symptoms such as boosted frequency, necessity, or leakage. Low levels of estrogen and urinary system incontinence work together. As females age and start approaching menopause, the ovaries reduce the process of making estrogen, and the levels of this female sex hormone normally decrease in the body. [newline] At some point, with menopause, the manufacturing of estrogen stops, and this influences the body in lots of methods. Without estrogen, females locate it difficult to preserve healthy and balanced urologic features during and after menopause. Bladder control for females starts together with their last menstruation period and enhances afterwards.Reduced Estrogen Levels
It can also deteriorate your pelvic floor muscular tissues, making it tougher to hold in urine. Nonneurogenic urinary incontinence may be brought on by structural or practical problems (e.g., ectopic ureters) impacting the storage phase of micturition. Hormone-responsive incontinence is also a typical kind of nonneurogenic urinary incontinence. In these people (generally pets), the detrusor reflex is regular; typical peeing habits, in addition to pee dribbling, happens.Just How Can I Lower My Risk Of Anxiety Incontinence?
It likewise helps keep your bladder and urethra healthy and balanced and operating properly. They might no longer be able to control your bladder as they did in the past. As your estrogen levels remain to drop throughout and after menopause, your UI signs might become worse. Estrogens, normally in the form of diethylstilbestrol, are carried out to purified females.- Endocervix glandular tissue activity during menopause and ultimately the amount of mucin decreases that this causes to vaginal dry skin that develops as a main issue in postmenopausal women.
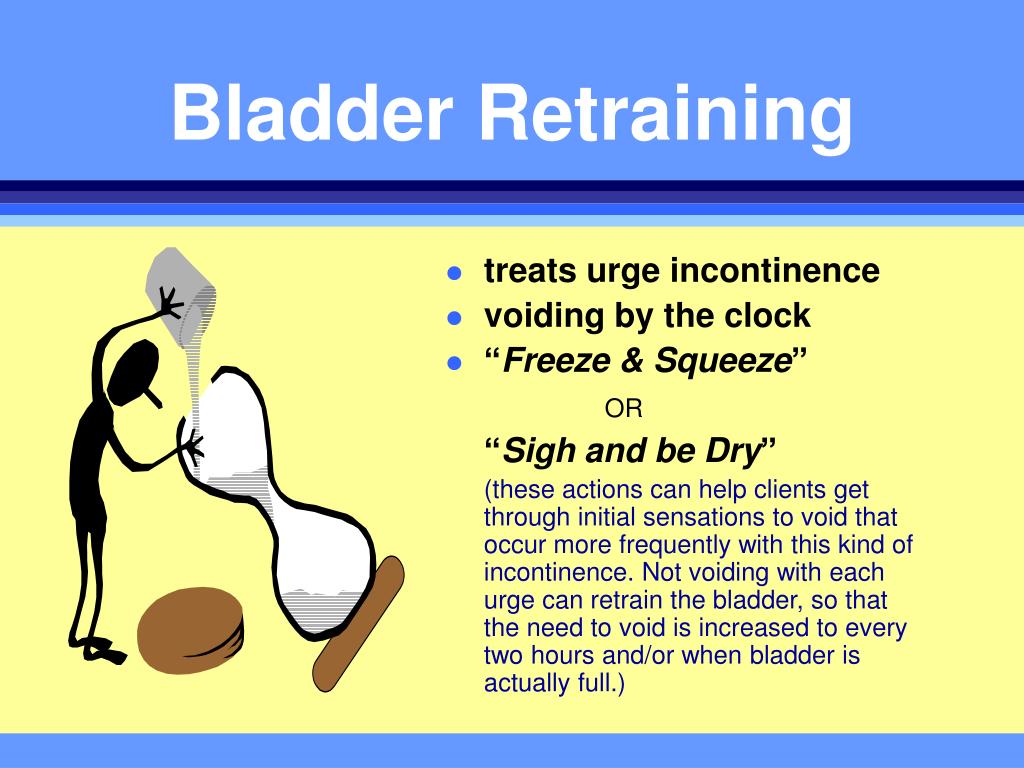
- Urge urinary incontinence is more prevalent after the menopause, and the height frequency of stress incontinence happens around the moment of the menopause.
- These hormone shifts can affect bladder feature and urinary system practices, showing up as urinary signs such as increased regularity, seriousness, or leakage.
- Anxiety incontinence creates when task places enhanced pressure on your bladder.
Which hormonal agent is accountable for bladder?

Social Links