September 3, 2024
Menopause And Urinary System Incontinence
Impacts Of Estrogen With And Without Progestin On Urinary Incontinence Geriatrics Jama From the age of puberty to menopause, hormone fluctuations can affect the stamina and function of the pelvic flooring muscles, commonly causing urinary problems such as anxiety urinary incontinence (SUI). A large component of this is because of maternity, childbirth and menopause. Each of these occasions in a female's life can lead to bladder control concerns. Pregnancy can be a short-term source of incontinence and the bladder control issues generally get better after the child is birthed. Some women experience urinary incontinence after shipment because of the strain giving birth takes on the pelvic flooring muscular tissues. When these muscles are deteriorated, you're most likely to experience leakage concerns. This sort of urinary incontinence causes you to leakage urine when you feel an urgent need to pee. Anxiety urinary incontinence is the most typical kind of urinary system incontinence. It can happen throughout exercise, coughing, giggling and sneezing. Pelvic flooring exercises (Kegels) can strengthen muscle mass and reduce signs. Some individuals require pessaries, bladder slings or various other treatments.Estrogen
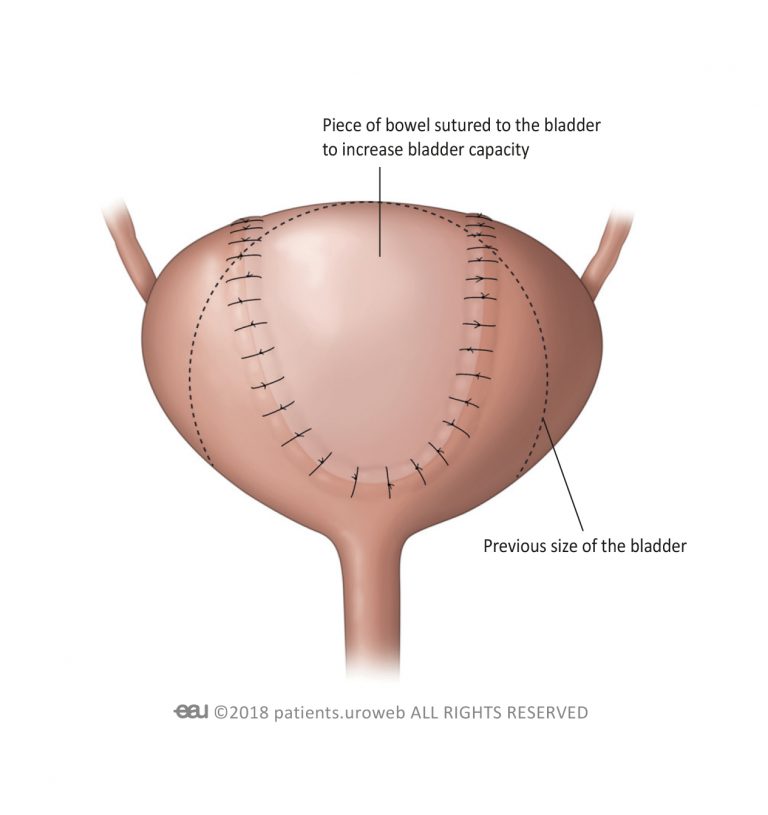
Furthermore, the individual relearns exactly how to manage the bladder and enhance the entailed muscular tissues. Urinary bladder hypocontractility or inadequate accommodation of pee throughout storage space may result in frequent leakage of tiny quantities of pee. Disorder may be brought on by urinary system infection, chronic inflammatory disorders, neoplastic sores, outside compression, and persistent partial outlet obstruction.Information From Mayo Center
In 1989, the National Institutes of Health Consensus Growth Conference estimated the yearly price of urinary incontinence in the USA to be $12.4 billion. True prices can be challenging to approximate because several individuals do not come to the attention of clinical specialists. Urinary urinary incontinence should not be thought of as a condition, because no particular etiology exists; most specific cases are likely multifactorial in nature. The etiologies of urinary incontinence vary and, oftentimes, incompletely comprehended. It is necessary to tell your medical professional or TENS Units registered nurse if you are having issues. Figure out if you qualify to get urinary incontinence products cost-free through your insurance policy at the end of the web page. An individual must talk with a doctor if they have any issues they may have reduced estrogen or if they are experiencing bladder signs. Reduced estrogen can additionally impact people outside of menopause, particularly after delivering or during breastfeeding. As many as 15% of premenopausal women might have GSM-like signs consequently. However, they can also go down during various other phases of life, such as after giving birth or while breastfeeding.- Double-contrast cystography may be shown for full visualization of the urinary bladder and identification of urinary bladder lesions.
- In psychophysiological feedback, a cable is connected to an electric spot over your bladder and urethral muscles.
- Prompt urinary incontinence is much more common after the menopause, and the top frequency of stress incontinence happens around the moment of the menopause.
- These hormonal shifts can affect bladder function and urinary practices, materializing as urinary system symptoms such as boosted regularity, necessity, or leakage.
- Stress urinary incontinence creates when activity places boosted stress on your bladder.
Exactly how can bladder leakage be quit?
and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and sleep issues.Digestive distress. Applying low-dose, topical estrogen may aid. The medicine comes in the type of a vaginal lotion, ring or patch. The estrogen may assist bring back the tissues in the vaginal canal and urinary tract to alleviate some signs. Topical estrogen may not be risk-free for people with a history of bust cancer cells, uterine cancer or both. Summary. Bladder dysfunction is an usual obstacle, particularly later on in life and throughout times of significant hormone adjustment. Low estrogen bladder signs can consist of urinary incontinence, over active bladder, and discomfort.

Social Links