September 3, 2024
Physiotherapy In Ladies With Urinary Incontinence

Medical Therapies For Women With Stress Urinary Incontinence: An Organized Evaluation Pmc User comments should remain in English, understandable and appropriate to the article controversial. We reserve the right to remove any remarks that we consider to be unsuitable, offending or otherwise in violation of the Individual Comment Terms and Conditions. When criticisms of the short article are based upon unpublished data, the information must be provided. Whilst Botox for Incontinence theoretically this is appealing, the invasive nature of the insertion of the gadgets may avoid them from being adopted in people. Additional study is required to optimise minimally invasive devices, concentrating on accuracy of measurements and acceptability to patients37. The European Association of Urology guidelines suggest UDS if the findings might affect the option of invasive treatment; it also recommends that UDS not be consistently offered for straightforward urinary incontinence or prior to treatment of pure SUI.
- A large evaluation found comparable results, and the continence rates for open Burch procedures were kept in mind to be 85% at 1 year postoperatively and roughly 70% after 5 years [31]
- This unroofing of the diverticulum changes the slim communication with the urethra that causes signs when it becomes obstructed into a wide-mouthed sac that drains pipes freely.
- All randomised studies deal with the constraint that people can not be blinded to the therapy allocation considering that all recruited people have to react to a test phase prior to randomisation.
- Females with MUI are less most likely to be cured of their UI by SUI surgery than women with SUI alone.
Client Education And Learning
The very same authors did a potential evaluation of 505 females who had POP surgical procedure with or without mesh [652] The incidence of aggravating urinary system regularity decreased from 36.6% to 14.6%, with de novo signs happening in 6.1%. Troublesome urgency symptoms decreased in 36.8% to 12.9% of females, with 5.0% developing afresh symptoms. Prompt urinary system incontinence signs and symptoms lowered from 21.2% to 6.1% of ladies, with 5.3% developing afresh signs and symptoms. A large RCT included females with POP without signs of SUI, that were randomised to sacro-colpopexy with or without Burch colposuspension [631] Three hundred and twenty-two stress-continent women with stages 2-- 4 prolapse undertook standardised urodynamic testing, and the protocol consisted of 5 prolapse decrease approaches.Mid-urethral Transobturator Tape Sling
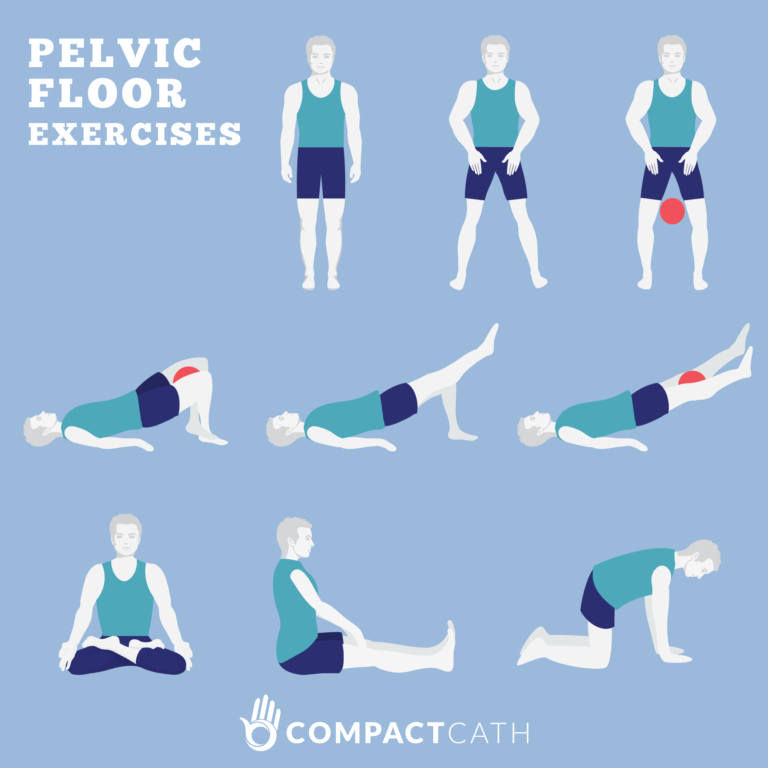
Pelvic floor muscle training is suggested as first‐line traditional monitoring for treating urinary incontinence. Added physical treatments, such as electric stimulation, biofeedback or magnetic stimulation can be considered in women who can not proactively get their pelvic floor muscle mass, in order to help motivation and adherence to treatment. Physio therapists need to comprehend the nature of the urinary system incontinence, the impact prognostic factors and the principal of treatment modalities.What is the very best therapy for urinary incontinence?
Social Links